Did you know…?
2 in 3 Australians (men and women) over 50 years old have osteoporosis or osteopenia1. Let me repeat that. Two in three Australians. This is the equivalent to picking two friends over 50 years old – between the three of you, two are likely to have (right now) weakened or brittle bones. Not only does this increase your fracture risk, but it can significantly impact your income, your quality of life and your independence.
Prevention is best.
Let’s look at women…
In 2012, 48.9% of women 50-69 had osteopenia (weak bones), and 12% had osteoporosis (brittle bones)1.
In 2012, 46.1% women over 70 had osteopenia (weak bones), and 43.2% had osteoporosis (brittle bones) 1.
Despite these staggering numbers, 8 out of 10 women do not feel personally at risk for the disease.
What is osteoporosis?
Osteoporosis occurs when bones lose minerals, such as calcium, more quickly than the body can replace them, leading to a loss of bone thickness (bone mass or density). As a result, bones become thinner and less dense, so that even a minor bump or fall can cause serious fractures. These are known as ‘fragility’ or ‘minimal trauma’ fractures.
Osteoporosis is often referred to as a ‘silent epidemic’. Generally speaking, there are no ‘warning signs’ or symptoms of osteoporosis with most cases of osteoporosis being diagnosed after the first fracture.
Osteoporotic fractures most commonly occur in the wrist, spine, hip and pelvis. As these fractures are often the result of a small bump, or light fall, people are often not aware of the severity of their injury. It is not unheard of for a fractured spine to be dismissed as age-related back pain.
What is osteopenia?
Osteopenia is a decrease in bone density and quality, but not to the extent of osteoporosis. A diagnosis or recognition of osteopenia is a warning sign that should look at possible lifestyle changes in order to prevent osteoporosis.
Unfortunately, more fractures occur in women whose bone mineral density has not fallen into the osteoporosis definition. One study that followed a random sample of postmenopausal women showed that the incidence of a fracture was highest in women with osteopenia (56%), followed by osteoporosis (25%)2.
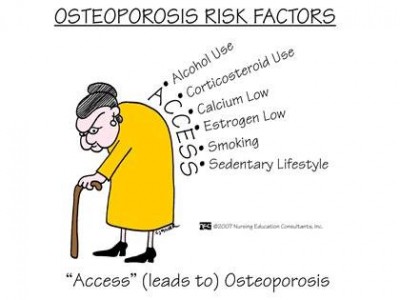
Risk Factors for Osteoporosis and bone fractures
Low bone mineral density
Bone mineral density (BMD) is a marker that is utilised for osteoporotic diagnosis and risk. Your BMD can be confirmed via a DEXA scan.
Post-menopausal women
Women are at a greater risk of developing osteoporosis than men. Women generally have smaller bones than men and also experience a rapid decline in the production of the hormone oestrogen during the menopause.
Oestrogen protects the bones; when oestrogen levels decrease, the bones lose calcium and other minerals at a much faster rate. As a result, bone loss of approximately 2% per year occurs for several years after menopause.
History of a prior fracture
It is believed that approximately 50% of people with one fracture due to osteoporosis will have another. Unfortunately, the risk of further fractures increases with each new fracture, creating a downwards spiralling ‘cascade effect’.
Family history of osteoporosis
Bone health has a strong genetic predisposition, so consider your family history of osteoporosis. If someone in your family has osteoporosis or osteopenia, it is particularly important to do what you can to prevent yourself from developing the condition.
Low Vitamin D status
Vitamin D plays an essential role for bone health. It promotes calcium absorption in the gut and maintains adequate calcium and phosphate levels in the blood. Vitamin D is needed for bone growth and bone remodelling, and together with calcium, helps to protect older adults from osteoporosis.
Low calcium levels
Calcium is essential for bone structure. Without structure, bones are weak and brittle.
Low body mass index (BMI)
Several studies have shown that a lower BMI is related to a higher risk of developing osteoporosis3, 4, 5. A BMI of less than 28 has been proposed as a potential indicator for osteoporosis risk4. BMI = weight (kg) / (height (m) x height (m))
Reduced physical activity / Sitting
A recent study of 2117 individuals showed that sedentary behaviour and sitting (time spent in non-exercising seated and reclining positions) has an increased risk, or association with a low bone mineral density of the hip and pelvis6.
Symptoms:
Unfortunately, there are no obvious symptoms for osteoporosis. Some subtle hints that indicate you may be a risk include:
- Getting shorter
- Breaking bones as a result of a small bump or fall
- Stooped posture (bent forwards)
What can I do?
- Ensure you are getting enough vitamins and minerals to build and strengthen your bones. These can be added to your diet, and/or added as a supplement. If you are considering a supplement, always talk to a professional first (talk to us about speaking to one of our naturopaths).
- Calcium
- Vitamin D
- Magnesium
- Vitamin K
- Boron
- Bring exercise into your routine
- Weight bearing exercise: With proper technique, and adequate supervision, weight bearing exercise can help to halt osteoporosis degradation.
- Balance exercise: Balance exercise can significantly help reduce the risk of falls, and thus reduce the risk of fractures from a fall.
- Consider bio-identical hormone replacement therapy during perimenopause and menopause.
- The sudden decline in oestrogen leaves your bones susceptible to a rapid decline in bone strength. Supplementing with oestrogen can delay and reduce this sudden change, potentially reducing your risk of developing osteoporosis.
If you have any questions, or you are after some support, please let us know by filling in the form to the right, or by calling us on 1300 883 405.
References:
- Watts JJ, Abimanyi-Ochom J, Sanders KM. Osteoporosis costing all Australian : a new burden of disease analysis – 2012 to 2022. Melbourne, Vic.: Osteoporosis Australia; 2013. 75 p.
- Pasco JA, Seeman E, Henry MJ, Merriman EN, Nicholson GC, Kotowicz MA. The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2006;17(9):1404-9.
- Kim MH, Lee JS, Johnson MA. Poor Socioeconomic and Nutritional Status Are Associated with Osteoporosis in Korean Postmenopausal Women: Data from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES) 2009. Journal of the American College of Nutrition. 2015;34(5):400-7.
- Jiang X, Good LE, Spinka R, Schnatz PF. Osteoporosis screening in postmenopausal women aged 50-64 years: BMI alone compared with current screening tools. Maturitas. 2016;83:59-64.
- Silva TR, Franz R, Maturana MA, Spritzer PM. Associations between body composition and lifestyle factors with bone mineral density according to time since menopause in women from Southern Brazil: a cross-sectional study. BMC endocrine disorders. 2015;15:71.
- Chastin SF, Mandrichenko O, Helbostadt JL, Skelton DA. Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone. 2014;64:254-62.